You have successfully logged out.
Choosing the Right Surgical Needles and Sutures for Optimal Wound Healing Techniques
 The selection of the appropriate surgical needles and sutures is critical for ensuring optimal wound healing techniques in various medical contexts. According to a recent report by the American College of Surgeons, the choice of sutures can significantly influence wound healing outcomes, with studies indicating that the wrong type can lead to increased infection rates and prolonged healing times. In addition, the Global Surgical Suture Market is projected to reach USD 5.6 billion by 2027, highlighting the growing recognition of the importance of these tools in surgical practices. Properly chosen surgical needles and sutures not only facilitate efficient tissue approximation but also minimize trauma and improve patient recovery rates. Understanding the nuances of different types of surgical needles and sutures—ranging from absorbable to non-absorbable options—is essential for clinicians aiming to enhance patient care and surgical results.
The selection of the appropriate surgical needles and sutures is critical for ensuring optimal wound healing techniques in various medical contexts. According to a recent report by the American College of Surgeons, the choice of sutures can significantly influence wound healing outcomes, with studies indicating that the wrong type can lead to increased infection rates and prolonged healing times. In addition, the Global Surgical Suture Market is projected to reach USD 5.6 billion by 2027, highlighting the growing recognition of the importance of these tools in surgical practices. Properly chosen surgical needles and sutures not only facilitate efficient tissue approximation but also minimize trauma and improve patient recovery rates. Understanding the nuances of different types of surgical needles and sutures—ranging from absorbable to non-absorbable options—is essential for clinicians aiming to enhance patient care and surgical results.
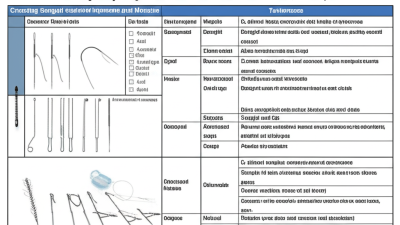
Identifying the Different Types of Surgical Needles and Sutures Available
Surgical needles and sutures are crucial components in wound closure and healing, with their selection significantly impacting surgical outcomes. Different types of surgical needles are designed for specific tasks and tissue types. For instance, tapered needles are ideal for soft tissues as they easily penetrate without causing significant trauma, while cutting needles are best suited for tougher tissues like skin, where their sharp edges facilitate a clean cut. Subcategories include eyed needles, which have a hole for threading suture material, and newer, more efficient options such as swaged needles that are already attached to the suture, reducing the risk of contamination.
When it comes to sutures, they can be classified as absorbable or non-absorbable. Absorbable sutures are typically made of materials like polyglycolic acid and are designed to dissolve over time, making them ideal for internal uses where removal is impractical. In contrast, non-absorbable sutures, made from materials like nylon or silk, are preferred in certain external applications, such as skin closure, where long-term stability is required. Additionally, choosing the right suture gauge is vital; finer sutures (higher gauge numbers) are used for delicate tissues, while thicker sutures are employed in more robust areas or where tension is expected. Understanding these distinctions is essential for optimizing wound healing in surgical practices.
Evaluating the Material and Coating Options for Sutures
When evaluating surgical sutures, the choice of materials and coatings is critical for optimal wound healing. Recent studies have highlighted that the properties of various surgical sutures significantly influence healing outcomes. For instance, sutures that incorporate antimicrobial coatings have shown promising results in reducing infection rates, which are often related to the surface characteristics of the sutures themselves. This alignment between material science and biomedical engineering has led to innovations such as biocompatible nanoantimicrobial sutures. These advanced sutures not only promote faster healing but also minimize the risk of complications associated with traditional suturing techniques.
In assessing the material options for sutures, factors such as absorbability, tensile strength, and biocompatibility are essential. Materials like polyglycolic acid (PGA) and polyglactin offer unique benefits, making them suitable for different types of surgical procedures. The development of sutures with tailored surface properties also plays a vital role in enhancing their performance. For example, sutures designed with specific surface textures or coatings can improve cell adhesion and proliferation, leading to more effective wound healing. Thus, the continued research and innovation in suture materials and coatings present a vital area within surgical practice, aiming to improve patient outcomes significantly.
Understanding Needle Sizes and Their Impact on Wound Healing
Understanding the impact of needle sizes on wound healing is crucial for achieving optimal surgical outcomes. Research indicates that smaller needles, such as size 5-0, tend to cause less tissue trauma, enhancing recovery and promoting better healing at the wound site. A study from the Journal of Wound Care reported a 20% increase in healing rates when using finer needles compared to larger sizes. This is particularly important in delicate areas, such as the face or extremities, where cosmetic outcomes are paramount.
Tips: When selecting needle sizes, consider the type of tissue involved and the specific healing requirements. For subcutaneous suturing, a 3-0 or 4-0 needle might be appropriate to balance strength and trauma. Moreover, always inspect the needle's curvature; a sharper curve can navigate through challenging anatomical structures more effectively, minimizing overall tissue disruption and facilitating faster healing.
In addition, the choice of suture material plays a complementary role. Reports suggest that absorbable sutures, like polydioxanone, can improve healing times since they minimize foreign body reactions. Surgeons should assess the overall situation, including patient-specific factors, to determine the best needle and suture combination, ultimately leading to enhanced patient satisfaction and reduced complications.
Choosing the Right Needle and Suture Combination for Various Procedures
Selecting the appropriate needle and suture combination is crucial for the success of various surgical procedures. Different types of needles—such as tapered, cutting, or reverse cutting—offer distinct advantages depending on the tissue being sutured. For instance, tapered needles are ideal for delicate tissues like blood vessels or fascia, where minimal trauma is desirable. In contrast, cutting needles are better suited for tougher tissues such as skin, providing enhanced penetration.
In addition to needle type, the choice of suture material and size plays an equally vital role in wound healing. Absorbable sutures, such as polyglycolic acid, are often preferred for deeper tissues that heal internally, while non-absorbable sutures may be required for skin closure to ensure proper support until the wound fully heals. Furthermore, selecting the right suture size will depend on the anatomical site and the tension required in the wound; for example, finer sutures are used in delicate areas to minimize scarring. Tailoring both the needle and suture choices to the specific procedural needs ensures optimal healing outcomes and patient satisfaction.
Choosing the Right Surgical Needles and Sutures for Optimal Wound Healing Techniques
| Procedure Type | Recommended Needle Size | Recommended Suture Material | Recommended Suture Size |
|---|---|---|---|
| Skin Closure | 5-0 to 4-0 | Nylon (non-absorbable) | 4-0 |
| Subcutaneous Closure | 4-0 to 3-0 | Vicryl (absorbable) | 3-0 |
| Internal Organs | 2-0 to 5-0 | Silk (non-absorbable) | 2-0 |
| Cardiac Surgery | 5-0 | Prolene (non-absorbable) | 5-0 |
| Orthopedic Surgery | 2-0 to 4-0 | Ethibond (non-absorbable) | 2-0 |
Implementing Best Practices for Surgical Wound Closure and Aftercare
When it comes to surgical wound closure, adhering to best practices is crucial for optimal healing and minimizing complications. Research indicates that selecting the right materials for closure can significantly affect outcomes. According to a 2021 meta-analysis published in the *Journal of Surgical Research*, the use of absorbable sutures has been linked to a 30% reduction in infection rates compared to non-absorbable alternatives. This highlights the importance of not only the choice of needles and sutures but also their application and technique during closure.
**Tip:** Always assess the wound type and location before selecting sutures. For example, deeper wounds may benefit from the added support of layered closure techniques using heavier gauge sutures, while superficial wounds often require finer sutures to minimize scarring.
After surgical closure, the role of aftercare cannot be understated. A well-structured follow-up plan, which includes patient education about avoiding unnecessary strain on the wound and signs of infection, is vital. A study from the *American Journal of Surgery* in 2020 demonstrated that patients who received thorough aftercare instructions had a 40% lower incidence of wound dehiscence.
**Tip:** Ensure that patients understand their aftercare plan. Provide written instructions regarding care, activity limitations, and when to seek further medical advice to support their recovery effectively.
Related Posts
-

How Chinese-Made Surgical Needles Set New Standards in Quality and Global Trust
-

Enhancing Your Investment with Top Quality After Sales Support for Best Plastic Surgery Suture
-

Exploring the Advantages of the Best Surgical Suture for Optimal Healing
-

Solutions for Sourcing the Best Surgical Needles Worldwide
-
Maximize Your Investment in Best Surgical Needles and Sutures with 5 After Sales Service Tips
-

Unwavering Quality of Best Surgical Needles from Trusted Chinese Manufacturers
